Vagina and Vulval Health The vagina is a closed muscular canal that extends from the the outside of the female genital area (vulvar) to the neck of the uterus (cervix). Various factors such as sex and your general health can affect the health of your vagina and vulvar. The vulva is the name given to the external female genital organs.
The vagina is a closed muscular canal that extends from the the outside of the female genital area (vulvar) to the neck of the uterus (cervix). Various factors such as sex and your general health can affect the health of your vagina and vulvar. The vulva is the name given to the external female genital organs.
Vaginal problems
At the top of the vulva is the mons pubis. Below the mons pubis there are two folds of skin called the labia majora (outer lips) and labia minora (inner lips).
The labia minora changes during puberty and often become more prominent. This is completely normal, like all of the other changes that take place during puberty. The appearance of the vulva continues to change throughout your life because of hormonal changes and age. The appearance of the vulva also varies between females.
Many women put up with vulvar discomfort, either because they are embarrassed and are not sure where to seek help. Many issues can be treated, others may need a long term plan to provide symptom relief. All symptoms or changes noticed in this part of the body should be checked by a medical professional to exclude uncommon but serious causes.
Vulvar problems
The skin in the vulval area is very sensitive and some women experience discomfort such as:
- itchiness
- burning sensation
- pain
- swelling
- lumps
- ulcers
- vaginal discharge
These symptoms can be caused by a range of conditions such as:
- allergy and hypersensitivity (soap, laundry detergent, toilet paper, sanitary pads, underwear)
- skin conditions (dermatitis, psoriasis)
- infections (thrush, genital herpes, genital warts)
- vulvodynia (pain in the vulva)
- pre-cancerous and cancerous conditions
- vulval varices (varicose veins)
If you do have any of these symptoms it is important to have a check-up so the problem can be diagnosed and treated.
For more information, please see the following fact sheets:
Vulval and vaginal health from True (PDF 174.4KB)
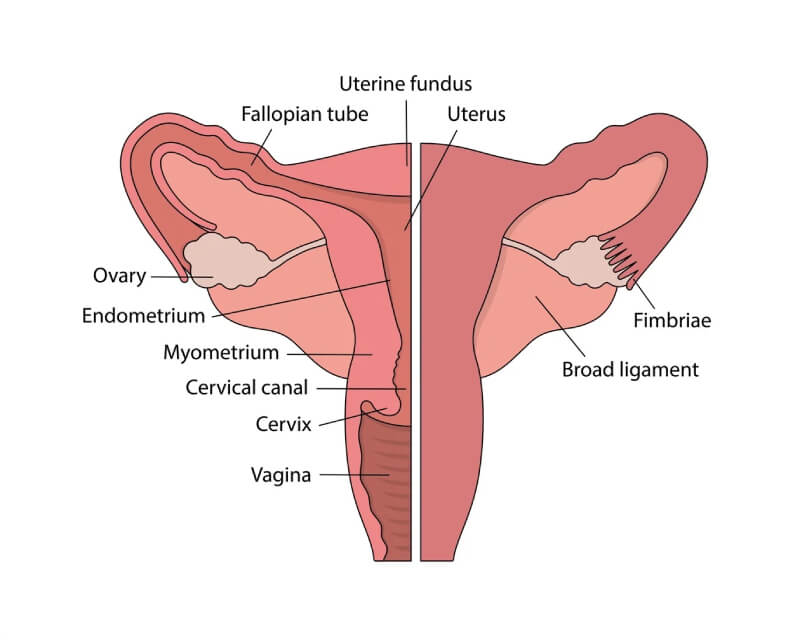
What is Cervical Screening?The cervix is often referred to as the ‘neck of the womb’ which sits at the inside end of the vagina. Cervix or Cervical cancer is a cancer of the cells of the cervix and is preventable. Cervical screening can detect changes in the cells of the cervix BEFORE they become cancerous.
Cervical screening
What is Cervix (Cervical) Cancer?
The cervix is often referred to as the ‘neck of the womb’ which sits at the inside end of the vagina.
Cervix or Cervical cancer is a cancer of the cells of the cervix and is preventable.
Cervical screening can detect changes in the cells of the cervix BEFORE they become cancerous.
The new Cervical Screening Test will prevent even more cancers
A cervical screening test (Pap test) is a simple test that checks for early changes to the cells of the cervix. These changes may lead to cervical cancer but having cervical screening significantly reduces this risk.
Regular cervical screening saves many lives each year from cervical cancer. About eighty percent of people who develop cervical cancer have not had regular cervical screening tests or have never had one.
The National Cervical Screening program (NCSP) is changing. Due to a better understanding of the Human Papilloma Virus (HPV) and its natural history, HPV school vaccination programs and availability of new technology, the program has been updated to further reduce the risk of cervical cancer in Australia.
The current system of having two yearly cervical screening is being replaced by HPV testing with cytology (if required) every five years. Using knowledge about the HPV types that cause cell changes, and new technology, we can now look for the virus with better accuracy than we could look for abnormal cells.
After 1 December 2017, anyone with a cervix and aged between 25 and 74 years who have been sexually active will be invited to attend cervical screening every five (5) years. This includes people who have had the HPV vaccine because the vaccine does not protect against all types of HPV. See HPV and HPV vaccinations for more information.
| |
New changes |
Before the changes |
| Cervical Screening test |
HPV testing
If HPV test positive, then liquid-based cytology is also performed |
Pap test (cytology) |
| Sample collection |
Using a speculum, cells are collected from the cervix |
Using a speculum, cells are collected from the cervix |
| Sample preparation |
Liquid-based cytology |
Pap smear slide or liquid-based cytology |
| Screening Interval |
Five years* |
Two years* |
| Age range for participation |
25-74 |
18-69 |
*if no abnormalities found
What will cervical screening involve?
During the procedure, which only takes a few minutes, the doctor or nurse gently inserts an instrument called a speculum into the vagina, so that the cervix can be seen. A tiny brush is then inserted into the vagina to collect cells from the cervix. These cells are added to a solution called liquid-based cytology (LBC) which is sent to the laboratory for HPV testing. The results are usually available within a couple of weeks. If HPV virus is detected, then the laboratory will report whether the cervical cells are normal or not.
This quick procedure might feel a bit uncomfortable, but it shouldn’t hurt. If it does hurt at any stage throughout the procedure tell the doctor/nurse immediately.
Occasionally, the laboratory will report that the sample was unsatisfactory and another cervical screen has to be taken. Usually, this is because not enough cells were collected. This doesn’t mean your cervical screening is abnormal, but more likely that the laboratory has received an insufficient amount of cells.
I’m under 25 years of age, why don’t I get offered screening anymore?
Evidence shows that:
- There are low rates of cervical cancer in this age group
- Before the introduction of the new cervical screening (HPV testing), cervical screening was not very effective in this age group at preventing cancer
- HPV vaccination programs have reduced the incidence of HPV in vaccinated and unvaccinated populations
- Most young persons will clear the HPV virus all by themselves
- Younger generations are at risk of overtreatment in the current cervical screening program
- More cervical cancers are predicted to be prevented using the new cervical screening program
However, it is important that you visit your local health care professional if you have symptoms such as unexpected vaginal bleeding or unusual discharge.
If you have any questions which aren’t answered here, email cervicalscreening@true.org.au or talk to your local health care professional.
To book a cervical screening test at one of our clinics, please go to https://www.true.org.au/clinic.
Abnormal cervical screening results:
Abnormal results will be reported in two stages; the first will about be the HPV virus being detected. The second result will whether or not there is an abnormality found in the cervical cells on the cervical screening test.
If the results of your cervical screen are abnormal this does not mean you have cancer. Often abnormal results are caused by an inflammation or infection that will clear up naturally. Sometimes you may need to have cervical screening more often.
The Pap test and the new HPV test can only screen for possible problems, not diagnose them. If your cervix appears abnormal during the pelvic examination or you have an abnormal test, your doctor may organise for you to have a colposcopy. A colposcopy is a simple procedure that is performed in a doctor’s office. The doctor uses a device called a Colposcope, which is large microscope that is positioned approximately 30cm from your vagina. A bright light on the end of the Colposcope allows the doctor to see the cervix more clearly. The procedure is painless and takes about 10 to 15 minutes.
If the doctor sees abnormal cells they will take a biopsy. A biopsy involves taking a sample of the abnormal cell tissue from the cervix. It is not usually painful but may be uncomfortable. The sample is sent to the laboratory for testing. When the results come back, your doctor will recommend either treatment, another colposcopy in the future, more frequent cervical screening or no further action may be necessary.
Some types of abnormal cells may require specialist treatment. Make sure you talk to your doctor, nurse or health worker about what is best for you.
For information about cervical cancer prevention and information in other languages, go to Cancer Screening Australia
For information about cervical cancer prevention in the LGBTIQ+ communities, go to LGBTIQ - PapScreen Victoria.
For information about cervical cancer prevention for Indigenous communities, go to Information about cervical screening for Aboriginal women.
For more general information, visit the Cancer Council.